
Medi-Cal To Covered California Enrollment Program
India-West Staff Reporter
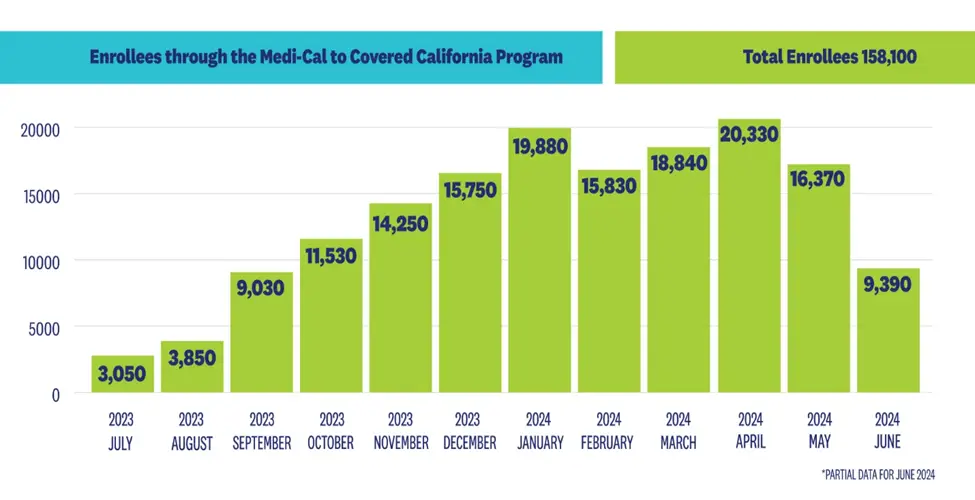
SACRAMENTO, CA — Covered California on June 11 announced that more than 158,000 Californians had remained covered through the Medi-Cal to Covered California enrollment program over the past year.
Beginning in April 2023, following the end of the federal continuous coverage requirement put in place during the COVID-19 pandemic, Medi-Cal resumed its renewal process by redetermining eligibility for over 15 million of its members. In May 2023, Covered California and the Department of Health Care Services (DHCS), which administers California’s Medi-Cal program, launched the Medi-Cal to Covered California enrollment program.
Under the program, Covered California automatically enrolls individuals in one of its low-cost health plans when they lose Medi-Cal coverage and gain eligibility for financial help through Covered California. Through early June of 2024, the program has helped 158,100 Californians remain insured.
“Through our partnership with DHCS, we have been able to help nearly 160,000 Californians seamlessly transition from Medi-Cal to Covered California and avoid gaps in coverage,” said Covered California Executive Director Jessica Altman. “We are proud of these results so far, and the Medi-Cal to Covered California program is now a mainstay in our effort to keep Californians covered with comprehensive, affordable health insurance.”
Many people who undergo the Medi-Cal renewal process may already have acquired another source of coverage — such as through a new job — and are no longer seeking insurance, but those who are without another source of coverage can turn to Covered California.
According to a survey conducted last fall on behalf of Covered California by NORC and Slosar Research, among the first month’s cohort of consumers automatically enrolled with Covered California following the loss of Medi-Cal eligibility, 82 percent report having coverage at the end of their special-enrollment period. That figure includes 31 percent reporting enrollment through Covered California.
While this 14-month redetermination period is ending, Medi-Cal’s normal redetermination process will continue, as will the Medi-Cal to Covered California program. Californians who are determined to no longer be eligible for Medi-Cal but who qualify for financial help through Covered California will receive information in the mail on their new Covered California plan. For eligible transitioning consumers, Covered California will automatically select a plan for the consumer that provides the most financial help.
Consumers can learn more about their options by visiting CoveredCA.com, where they can easily find out if they qualify for financial help and see the coverage options in their area or call (800) 300-1506.



